The TCA cycle constitutes the central biochemical hub of aerobic metabolism, operating within mitochondria to sequentially oxidize acetyl-CoA to carbon dioxide via enzymatic transformations. This process yields NADH, FADH₂, and GTP as energy carriers. Subsequently, these electron carriers fuel ATP synthesis via the ETC and oxidative phosphorylation, serving as the primary energy currency for cellular activities. This review provides a comprehensive analysis of TCA cycle enzymes, encompassing their roles, allosteric control, reaction kinetics, and biotechnological implications.
Citrate Synthase
Citrate synthase serves as the initiating enzyme in the TCA cycle, facilitating the condensation of acetyl-CoA and oxaloacetate to form citrate. During this reaction, the methyl group of acetyl-CoA binds to the carbonyl group of oxaloacetate, synthesizing citrate while releasing coenzyme A (CoA). This step is pivotal in cellular energy metabolism, marking the commencement of ATP generation and establishing the substrate framework for subsequent TCA cycle reactions.
Catalytic Mechanism
The enzyme orchestrates a multi-step process where acetyl-CoA and oxaloacetate undergo stereospecific binding. The methyl carbon of acetyl-CoA aligns with the carbonyl carbon of oxaloacetate, forming citrate through nucleophilic attack and subsequent hydrolysis. This exergonic reaction consumes one water molecule and liberates CoA, positioning citrate synthase as the gatekeeper of the TCA cycle. Its activity directly governs cellular energy flux by determining cycle initiation efficiency.
 Metabolic Pathway of Succinic Acid Production by Citrate Synthase (gltA) (Mutyala S et al., 2023)
Metabolic Pathway of Succinic Acid Production by Citrate Synthase (gltA) (Mutyala S et al., 2023)
Regulatory Mechanisms
Citrate synthase activity is modulated by several interconnected factors:
- Allosteric Suppression: Elevated intracellular ATP, NADH, or succinyl-CoA levels—indicators of energy surplus—bind to citrate synthase, inducing conformational changes that reduce substrate affinity. This feedback inhibition prevents excessive energy production during metabolic abundance.
- Substrate Limitation: Oxaloacetate availability critically influences reaction velocity. Diminished oxaloacetate concentrations lower enzymatic turnover, thereby throttling citrate synthesis. Conversely, substrate accumulation accelerates cycle progression.
- Energy Demand Sensing: Cellular AMP/ATP ratios indirectly regulate enzyme activity by modulating upstream pathways that supply acetyl-CoA and oxaloacetate.
Biotechnological Applications
As a linchpin in industrial biotechnology, citrate synthase is engineered to optimize citric acid biosynthesis in microbial cell factories. Strategies include:
- Citrate Synthase Dysregulation in Alzheimer's Disease: mitochondrial metabolic collapse and therapeutic potential of citrate in restoring acetylcholine synthesis. For example, Alzheimer's disease (AD) is marked by reduced citrate synthase (CS) activity in brain tissue and peripheral cells, impairing mitochondrial citrate and acetyl-CoA synthesis. This metabolic disruption diminishes acetylcholine (ACh) production, exacerbating cognitive decline. Citrate supplementation may counteract AD progression by restoring energy metabolism, enhancing ACh synthesis, and inhibiting amyloid-β aggregation. Concurrently, oxidative stress during AD's silent phase upregulates GLUT3 (enhancing glucose uptake) and PDK3 (inhibiting pyruvate dehydrogenase), further limiting acetyl-CoA availability and citrate formation. Targeting PDK3 to alleviate acetyl-CoA deficits and mitochondrial dysfunction may offer therapeutic promise, alongside behavioral interventions (e.g., intermittent fasting) to mitigate oxidative stress and improve mitochondrial quality control (Chhimpa N et al., 2023).
- Metabolic Balancing: Harmonizing key enzyme activities enhances process efficiency and product purity in biomanufacturing. For example, by regulating the activity of citrate synthase (GltA) instead of directly knocking out genes, the metabolic flow of acetyl coenzyme A can be balanced. It is found that reducing GltA activity can reduce the loss of acetyl coenzyme A entering TCA cycle, thus enhancing its flux towards 3-HB synthesis. This strategy combined over-expressed thiolase (PhaA) and NADPH-dependent acetoacetyl-CoA reductase (PhaB), which significantly increased the yield of 3-HB. Under the condition of glucose as the sole carbon source, the transformed strain E.coli ldhapoxbpta-ackaglta:: glta [A267t] achieved efficient synthesis of 3-HB (21.3 g/L effective concentration) through repeated batch process of phosphate starvation. The results verify the feasibility of the application of metabolic control strategy in industrial scale (Rajpurohit H et al., 2024).
Integration with Cellular Physiology
Beyond energy metabolism, citrate synthase interfaces with lipid synthesis, nitrogen assimilation, and redox homeostasis. Its product, citrate, acts as a mitochondrial-cytosolic shuttle for acetyl units, linking carbohydrate oxidation to fatty acid biosynthesis. Dysregulation of citrate synthase is implicated in metabolic disorders, underscoring its therapeutic relevance.
Aconitase
Aconitase facilitates the second catalytic step in the TCA cycle, converting citrate to isocitrate via a two-step isomerization process. Initially, citrate undergoes dehydration to form the intermediate cis-aconitate, which is subsequently rehydrated to yield isocitrate. This reaction is critical for maintaining TCA cycle flux, ensuring efficient energy production and metabolic continuity in cells.
Catalytic Mechanism
The enzyme operates through sequential transformations:
- Dehydration: Citrate loses a water molecule, forming cis-aconitate.
- Hydration: cis-Aconitate incorporates a water molecule to produce isocitrate. Central to this mechanism is the enzyme's reliance on a [4Fe-4S] iron-sulfur cluster, which stabilizes the active site and mediates electron transfer during substrate binding and catalysis.
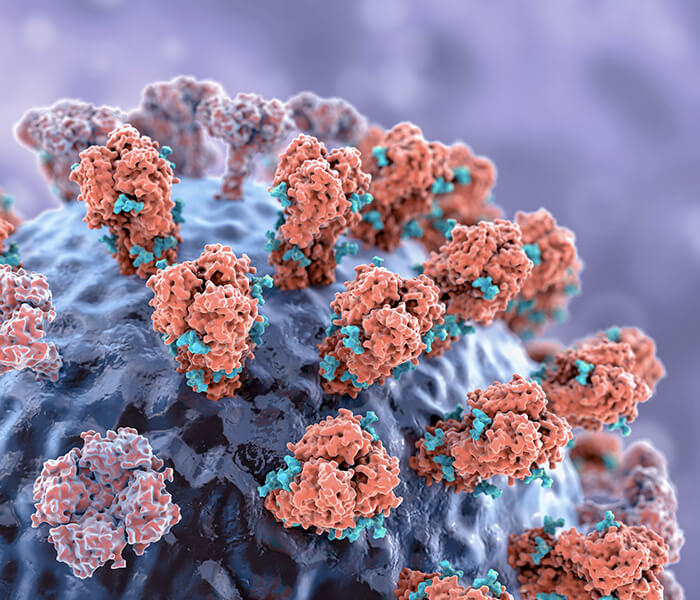
 Aconitase engagement in the TCA cycle (Padalko V et al., 2024).
Aconitase engagement in the TCA cycle (Padalko V et al., 2024).
Iron-Sulfur Cluster Dependency
Aconitase's [4Fe-4S] cofactor is indispensable for its activity. This cluster maintains the enzyme's structural integrity and facilitates substrate positioning. Disruption of the cluster—through oxidative damage, radical species, or iron depletion—compromises enzymatic function, stalling the TCA cycle and impairing cellular energy metabolism.
Regulatory Mechanisms
- Redox Sensitivity: Oxidative stress destabilizes the [4Fe-4S] cluster, converting aconitase into an inactive [3Fe-4S] form. Cellular antioxidant systems (e.g., glutathione) mitigate this inactivation by preserving cluster integrity.
- Iron Homeostasis: Intracellular iron availability modulates enzyme activity. Excess iron promotes oxidative cluster damage, while deficiency impedes cluster assembly, both impairing catalysis.
- Allosteric Modulation: Elevated ATP or NADH levels inhibit aconitase, aligning TCA cycle activity with cellular energy status to prevent metabolic overload.
Applications
- Cancer Therapeutics: Targeting iron metabolism in cancer cells via aconitase modulation offers potential strategies to disrupt tumor growth and metastasis. For example, It was found that the expression of mitochondrial aconitase (ACO2) in gastric cancer was significantly down-regulated, and the low expression was positively correlated with tumor progression (clinical stage, T/N/M grade, differentiation degree) and shortened survival time of patients. Multivariate analysis showed that ACO2 was an independent prognostic factor, which indicated that ACO2 might affect the occurrence and development of gastric cancer by regulating the cyclic metabolism of tricarboxylic acid, and it had the potential as a prognostic biomarker (Wang P et al., 2013).
- Dynamic transformation of iron and sulfur clusters and regulation of metabolic homeostasis. For example, As the key iron-sulfur enzyme in TCA cycle of Staphylococcus aureus, aconitase [4Fe-4S] cluster maintains catalytic activity and supports energy metabolism when iron is sufficient. However, under iron deficiency or oxidative stress, iron-sulfur clusters disintegrate, which leads to enzyme inactivation. Through the synergistic regulation of iron-free CitB(apo-CitB) and small RNA IsrR, apo-CitB inhibits circulating flux to prevent citric acid accumulation, while IsrR forms negative feedback by blocking the translation of transcription factor CcpE, which dynamically balances the metabolic network. This dual regulatory mechanism not only responds to iron starvation stress, but also reshapes metabolism to adapt to the host environment, ensuring the survival and virulence of pathogens (Barrault M et al., 2024).
- Reversible transformation of iron and sulfur clusters and stress response. For example, AcnA is the core metabolic enzyme of iron-sulfur cluster of Mycobacterium tuberculosis, which maintains its basic function under normal conditions, but its iron-sulfur cluster dissociates to form apo-AcnA under oxidation/nitrosation stress or iron starvation. Inactivated apo-AcnA dynamically regulates the phosphorylation level of peptidoglycan synthesis regulator CwlM (containing IRE-like sequence) to balance cell wall synthesis: under stress conditions, the toxic accumulation of nonphosphorylated CwlM is inhibited by AcnA; After the stress was relieved, AcnA restored the normal translation and function of CwlM through iron-sulfur cluster reconstruction. The IRE sequence of CwlM is a key regulatory site, and its destruction will lead to the accumulation of nonphosphorylated CwlM and weaken the resistance of bacteria to stress in host macrophages. This AcnA-CwlM regulatory axis has become the key mechanism of environmental adaptation and pathogenesis of Mycobacterium tuberculosis by integrating iron metabolism and cell wall homeostasis (Bancroft PJ et al., 2020).
Services You May Be Interested In
Additional Resources:
Isocitrate Dehydrogenase (IDH)
Catalytic Function
IDH catalyzes a two-step oxidative decarboxylation in the TCA cycle:
- Oxidation: Isocitrate is dehydrogenated to oxalosuccinate, with NAD⁺ or NADP⁺ serving as electron acceptors to yield NADH or NADPH.
- Decarboxylation: Oxalosuccinate loses a CO₂ molecule, forming α-ketoglutarate (α-KG). This reaction is pivotal for energy metabolism, generating NADH for ATP synthesis via oxidative phosphorylation. The product, α-KG, serves as a metabolic hub, linking the TCA cycle to nitrogen assimilation, amino acid biosynthesis, and epigenetic regulation.
Mechanistic Overview
IDH operates through a sequential mechanism:
- Substrate Binding: Isocitrate and NAD(P)⁺ bind to the enzyme's active site.
- Oxidative Decarboxylation: A hydride transfer from isocitrate to NAD(P)⁺ produces oxalosuccinate, followed by CO₂ release to form α-KG. The reaction strictly requires NAD⁺/NADP⁺ as cofactors, coupling substrate oxidation to cellular redox balance and energy production.
Regulatory Dynamics
IDH activity is tightly controlled by cellular energy status:
- Allosteric Activation: Elevated ADP (signaling energy deficit) and Ca²⁺ (indicating metabolic demand) enhance enzymatic turnover, amplifying α-KG synthesis to boost ATP generation.
- Feedback Inhibition: High ATP/NADH levels suppress IDH via negative feedback, preventing excessive TCA cycle flux and aligning energy output with cellular reserves. This dual regulation ensures metabolic flexibility, enabling cells to adapt to fluctuating energy requirements.
IDH Mutations in Oncogenesis
Somatic IDH mutations are implicated in gliomas and acute myeloid leukemia (AML). Wild-type IDH produces α-KG, whereas mutant isoforms (e.g., IDH1/2 R132H) catalyze isocitrate reduction to the oncometabolite D-2-hydroxyglutarate (2HG). 2HG disrupts epigenetic regulation by inhibiting α-KG-dependent dioxygenases, altering DNA/histone methylation patterns. This drives tumorigenesis by promoting hypermethylation phenotypes, genomic instability, and oncogenic signaling. Mutant IDH is a biomarker and therapeutic target, with inhibitors under development to block 2HG production and restore metabolic-epigenetic homeostasis (Liu S et al., 2020)
α-Ketoglutarate Dehydrogenase Complex (KGDH)
The KGDH is a pivotal enzyme assembly within the TCA cycle, catalyzing the oxidative decarboxylation of α-ketoglutarate (α-KG) to succinyl-CoA. This reaction generates NADH and CO₂, contributing to cellular energy production and metabolic homeostasis.
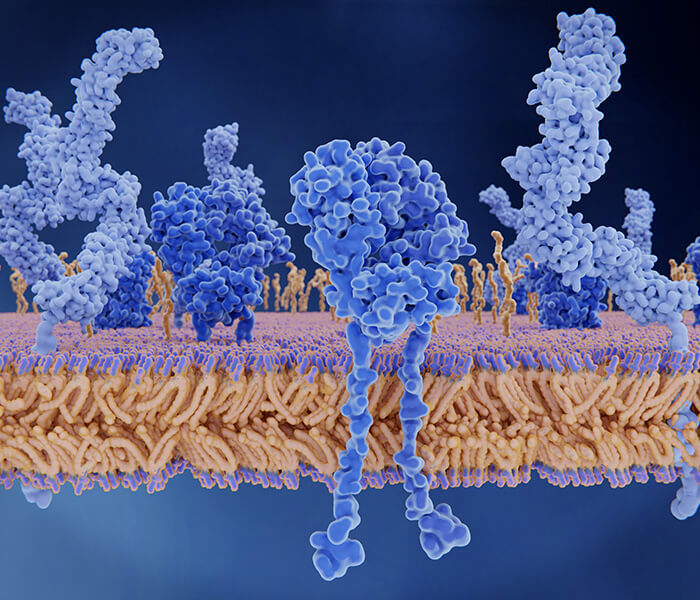
 Metabolic plasticity of the α-ketoglutarate dehydrogenase complex (KGDHC) (Hansen GE et al., 2020).
Metabolic plasticity of the α-ketoglutarate dehydrogenase complex (KGDHC) (Hansen GE et al., 2020).
Catalytic Mechanism
KGDH operates through a multi-enzyme process involving three core subunits and essential cofactors:
- E1 (α-Ketoglutarate Dehydrogenase): Initiates oxidation and decarboxylation of α-KG, utilizing thiamine pyrophosphate (TPP) as a cofactor.
- E2 (Dihydrolipoyl Succinyltransferase): Transfers the reaction intermediate to coenzyme A (CoA), forming succinyl-CoA.
- E3 (Dihydrolipoyl Dehydrogenase): Regenerates oxidized lipoamide via FAD and NAD⁺, producing NADH.
Cofactors
- TPP: Facilitates decarboxylation.
- CoA: Essential for succinyl-CoA synthesis.
- NAD⁺/FAD: Electron carriers critical for redox reactions.
- Lipoic Acid: Shuttles intermediates between enzyme subunits.
Regulatory Dynamics
KGDH activity is tightly regulated to align with cellular energy status:
- Negative Feedback Inhibition: Succinyl-CoA and NADH suppress activity to prevent metabolic overload.
- Calcium Activation: Elevated cytosolic Ca²⁺ in muscle cells enhances KGDH function, linking energy production to physiological demands.
Clinical and Therapeutic Relevance
- Neurodegenerative Diseases: neurodegenerative driving mechanism of energy metabolism collapse and protein's post-translation modification imbalance. For example: The impaired function of α -ketoglutarate dehydrogenase complex (KGDHC) drives neurodegenerative diseases through two paths: the inactivation of its catalytic subunit (such as DLST) leads to the inhibition of α -ketoglutarate oxidation, the reduction of succinic acid and succinyl -CoA production, which directly weakens the productivity and efficiency of mitochondrial oxidative phosphorylation; At the same time, the lack of succinyl -CoA damages protein succinylation modification, a key metabolic regulation mechanism, and further damages the cell homeostasis. Studies have confirmed that targeted inhibition of KGDHC activity or succinic acid metabolism can reproduce the phenotype of neuronal energy failure, and restoring KGDHC function may become the therapeutic target to reverse metabolic defects, and provide intervention strategies for neurodegenerative diseases such as Alzheimer's disease and Parkinson's disease(Piroli GG et al., 2023).
- Metabolic Syndrome: Dysregulation of KGDH may contribute to obesity and diabetes, highlighting its role in systemic metabolic health. For example, KGDH is the main source of mitochondrial hydrogen peroxide (mH2O2) production in mouse liver, and its mechanism of producing reactive oxygen species is directly related to the substrate metabolic state (such as the Krebs cycle initiated by malic acid when fatty acids are oxidized), instead of relying on the electron leakage of traditional electron transport chain complex I/III. KMV, a KGDH-specific inhibitor, can almost completely block mH2O2 production, while the complex I/III inhibitor has a weak effect, and its core role is the same in both sexes. In addition, KGDH maintains the balance between energy metabolism and redox by regulating the production of NADH/NADPH; Its abnormal function can lead to metabolic disorder, promote insulin resistance and fat accumulation, and become the key node of oxidative stress and energy imbalance in metabolic syndrome. This discovery provides a new direction for analyzing the interaction mechanism between oxidative damage and energy homeostasis in metabolic diseases (Grayson C et al., 2024).
- Redox regulation: metabolic remodeling of NAD(P)H and maintenance of redox homeostasis under oxidative stress. For example, in the oxidative stress induced by H2O2, aconitase is highly sensitive to low concentration H2O2 (≤ 50μ m) and completely inactivated. At this time, glutamic acid is used as a substitute substrate to maintain local NAH production in Krebs cycle and delay energy collapse. High concentration of H2O2 (≥ 100μ m) partially inhibited α -ketoglutarate dehydrogenase (α-KGDH) and reduced oxidative damage by limiting NADH accumulation. At the same time, the transformation from NADH to NADPH is enhanced, which promotes the removal of H2O2 and dynamically balances the reduction equivalent pool. This two-enzyme hierarchical regulation mechanism (aconitase as the initial sensitive target and α-KGDH as the core node of NADH steady state) cooperatively maintains the redox steady state, revealing the dynamic plasticity of metabolic pathways in stress adaptation (Tretter L et al., 2000).
Succinyl-CoA Synthetase (SCS)
SCS plays an essential role in the TCA cycle by catalyzing the conversion of succinyl-CoA to succinate, coupled with the synthesis of energy-rich phosphate compounds (GTP or ATP). This reaction is critical for cellular energy production and metabolic equilibrium, ensuring efficient ATP generation and cycle progression.
Catalytic Mechanism
SCS facilitates a two-step substrate-level phosphorylation process:
- Thioester Bond Cleavage: Hydrolysis of succinyl-CoA's high-energy thioester bond releases succinate and CoA, liberating energy stored in the bond.
- Nucleotide Phosphorylation: The liberated energy drives the phosphorylation of GDP or ADP to form GTP or ATP, respectively.
The resulting succinate re-enters the TCA cycle, where it is oxidized by succinate dehydrogenase to yield FADH₂—a key electron donor for the ETC—ultimately contributing to ATP synthesis.
Regulatory Mechanisms
SCS activity is modulated through multiple pathways to align with cellular demands:
- Substrate Availability: Elevated succinyl-CoA concentrations enhance enzymatic turnover, directly influencing reaction velocity.
- Energy Feedback:
- Inhibition: High ATP/GTP levels suppress SCS via feedback inhibition, preventing energy surplus.
- Activation: Increased ADP/GDP concentrations stimulate activity, prioritizing ATP/GTP synthesis during energy deficits.
- Post-Translational Modification: Phosphorylation by specific kinases or dephosphorylation by phosphatases dynamically regulates SCS activity, linking enzyme function to cellular signaling pathways.
- Isoenzyme Diversity: Tissue-specific SCS isoforms exhibit distinct kinetic properties and regulatory sensitivities, tailoring TCA cycle flux to meet organ-specific metabolic needs.
Physiological Implications
- Energy Homeostasis: SCS bridges catabolic and anabolic pathways, balancing ATP synthesis with biosynthetic precursor supply. For example, The forebrain-specific Sucla2 knockout mouse model constructed by CamKIIα α promoter successfully simulated the phenotype of human SCS deficiency (such as methylmalonuria and the increase of C3/C4-DC acyl carnitine), but there was no depletion of mtDNA in brain tissue, suggesting phenotypic tissue specificity. SUCLA2 deletion leads to the down-regulation of α(SUCLG1) and β(SUCLG2) subunits of SCS complex and the loss of function, and also leads to extensive succinylation modification of mitochondrial proteins. Compensatory mitochondrial proliferation (increased mtDNA content and up-regulation of 32% mitochondrial genes) and changes in chromatin accessibility (possibly transcription reprogramming mediated by histone succinylation) reveal the dual roles of succinylation modification in energy metabolism defects and epigenetic regulation (Lancaster MS et al., 2023).
- Disease Relevance: Dysregulation of SCS is implicated in metabolic disorders, underscoring its role in maintaining mitochondrial function. For example, SUCLG2, as a key enzyme of tricarboxylic acid cycle, catalyzes succinyl-CoA to generate GDP and drives TCA cycle oxidation reaction. Its deficiency leads to the transformation of T cell metabolism to reduction state, and abnormal accumulation of α-ketoglutaric acid, citric acid and acetyl coenzyme A(AcCoA), which promotes the differentiation of T cells into pro-inflammatory phenotype. In rheumatoid arthritis (RA), the increase of AcCoA level induces tubulin acetylation, stabilizes microtubule skeleton, promotes mitochondrial perinuclear localization, enhances T cell polarization, pseudopodia formation and tissue invasion, and aggravates inflammatory injury. By supplementing SUCLG2 or knocking out microtubule acetyltransferase to inhibit acetylation modification, abnormal migration of T cells and synovitis can be effectively blocked, and the regulatory pivotal role of metabolic-cytoskeleton dynamic interaction in autoimmune diseases can be revealed (Wu B et al., 2020).
Succinate Dehydrogenase (SDH)
Functional Role
SDH serves dual roles as both a TCA cycle enzyme and a core component of mitochondrial Complex II. It catalyzes the oxidation of succinate to fumarate, coupling this reaction to electron transfer for ATP synthesis. SDH uniquely bridges the TCA cycle and mitochondrial ETC, mediating energy production and redox homeostasis.
Catalytic Mechanism
The enzyme operates through three coordinated steps:
- Oxidation of Succinate: SDH abstracts hydrogen atoms from succinate, forming a transient double bond to generate fumarate. This reaction reduces the enzyme-bound FAD cofactor to FADH₂.
- Electron Shuttling: FADH₂ transfers electrons to ubiquinone (CoQ) via Complex II, feeding them into the ETC at Complex III (cytochrome bc₁ complex) to drive ATP synthesis.
- Metabolic Continuity: Fumarate re-enters the TCA cycle, undergoing hydration to malate for subsequent oxidative steps.
Regulatory Mechanisms
SDH activity is dynamically tuned to cellular metabolic states:
- Redox Coupling: High FADH₂/FAD ratios inhibit SDH via product feedback, preventing excessive succinate oxidation. Low FADH₂ levels enhance enzyme activity, prioritizing succinate flux during energy demand.
- Substrate-Driven Activation: Elevated succinate concentrations increase catalytic turnover, sustaining TCA cycle progression.
- Feedback Inhibition by Metabolites:
- Fumarate Accumulation: Suppresses SDH to prevent substrate overload.
- ATP/NADH Inhibition: High energy charge reduces SDH activity, aligning TCA flux with ATP sufficiency.
Pathophysiological Relevance
- Mitochondrial Disorders: SDH dysfunction disrupts ATP synthesis and redox balance, contributing to metabolic myopathies. For example, the lack of succinate dehydrogenase (SDH) activity in acute myeloid leukemia (AML) leads to succinate accumulation, which enhances cullin-mediated ubiquitination network by activating UBC12 phosphorylation, stabilizes oncogenes and relieves protein toxicity stress, thus enhancing the drug resistance of malignant cells to chemotherapy drugs. P-UBC12/cullin axis can reduce the sensitivity of treatment by regulating drug efflux pump and DNA repair mechanism, and the increase of succinic acid level can be used as a non-invasive marker of AML stratification. Targeted inhibition of succinic acid metabolism can reverse the drug resistance of SDH-deficient cells, significantly improve the low-dose efficacy of fludarabine and other nucleoside analogues, and provide a new strategy for precise treatment of AML (Chen Y et al., 2024).
- Cancer Metabolism: Mutations in SDH subunits (e.g., SDHB, SDHD) drive pseudohypoxia and tumorigenesis by stabilizing HIF-1α under normoxic conditions. For example, two kinds of succinate dehydrogenase isoenzymes (Sdh1/Sdh2) in MC²155 in mycobacterium smegmatis showed functional differentiation: Sdh1 was encoded by five gene operon, and Sdh2 was encoded by four gene clusters, which were differentially up-regulated under carbon restriction and hypoxia conditions. Gene knockout showed that the strain Δsdh2 had serious growth defects in various carbon sources, indicating that Sdh2 was an essential enzyme for core metabolism, while Δsdh1 had a normal phenotype. The competitive inhibitor 3- nitropropionic acid (3NP) can completely inhibit SDH activity-3NP treatment leads to the disappearance of membrane potential of wild-type and δ SD H1 strains during hypoxia, which proves that Sdh2 is the main driver of proton power in anoxic environment; However, under aerobic conditions, the membrane potential is not affected by 3NP, suggesting that there are other energy coupling mechanisms (Pecsi I et al., 2014).
Fumarase
Fumarase (fumarate hydratase) is a critical enzyme in the TCA cycle, catalyzing the stereospecific hydration of fumarate to malate. This reversible reaction ensures cycle continuity and intersects with biosynthetic pathways, influencing energy production, redox balance, and carbon flux.
Catalytic Mechanism
The enzyme facilitates fumarate hydration through a three-step process:
- Substrate Binding: Fumarate docks into the enzyme's active site, stabilized by electrostatic interactions with conserved residues (e.g., histidine, aspartate).
- Hydration: A water molecule, activated by the catalytic site, attacks the double bond of fumarate, forming a transient enol intermediate.
- Product Release: The intermediate tautomerizes to malate, which dissociates from the active site, enabling subsequent TCA cycle reactions.
- Fumarase achieves catalytic precision via its conserved active site architecture, which positions substrates for optimal stereochemical control.
Regulatory Dynamics
Fumarase activity is modulated by multiple factors:
- Substrate Availability: Elevated fumarate concentrations enhance enzymatic turnover, accelerating malate synthesis to sustain TCA cycle flux.
- pH Sensitivity: Maximal activity occurs near physiological pH (6.5–7.5), with deviations altering protonation states of catalytic residues, impairing function.
- Cofactor Dependence: Mg²⁺ ions stabilize the active site, promoting substrate binding and transition-state stabilization.
- Thermal Stability: Activity peaks at ~37°C; excessive heat denatures the enzyme, while lower temperatures reduce kinetic efficiency.
Biological and Clinical Significance
- Disease Associations: For example, hereditary leiomyomatosis and renal cell carcinoma (HLRCC) are driven by inactivation of fumarate hydratase (FH), and their related renal cell carcinoma (type 2) is resistant to radiotherapy, chemotherapy and immunotherapy. It is found that FH deficiency (FH⁻/⁻) and iron death inducer have a synthetic lethal effect: FH inactivation leads to fumaric acid accumulation, and the activity of key anti-iron death factor GPX4 is inhibited by post-translation modification, which makes tumor cells (such as UOK262) highly sensitive to iron death. Iron death inducer can selectively kill FH-deficient tumors and provide a new targeted therapy strategy for refractory cancers such as HLRCC (Kerins MJ et al., 2018).
- Biotechnological Applications: Engineered fumarase variants are employed in industrial malate production for food preservation and pharmaceutical synthesis. For example, recombinant strains such as Rhizopus oryzae and Escherichia coli are used to optimize metabolic pathways, tools such as CRISPR-Cas9 and RNA interference are used to target gene editing, glyoxylic acid cycle is introduced into Aspergillus oryzae to enhance precursor supply, and fumarate biosynthesis pathway is developed to improve economy. Although the yield of existing engineering strains is still lower than that of natural high-yield strains, the integration of multi-dimensional genetic modification is expected to promote the industrialization of bio-based fumaric acid production (Sebastian J et al., 2019).
Malate Dehydrogenase (MDH)
MDH is a pivotal oxidoreductase in eukaryotic and prokaryotic systems, orchestrating the interconversion of malate and oxaloacetate across metabolic pathways. It operates in both mitochondrial TCA cycle and cytosolic gluconeogenesis, coupling malate oxidation to NAD⁺ reduction, thereby linking carbon flux with cellular redox homeostasis.
Catalytic Mechanism
MDH facilitates a reversible, NAD⁺-dependent reaction through three coordinated stages:
- Substrate Docking: Malate binds to the enzyme's active site, stabilized by ionic interactions with conserved residues (e.g., arginine, histidine).
- Oxidative Decarboxylation: A hydride ion is abstracted from malate's α-carbon, transferring electrons to NAD⁺ to form NADH, while malate is dehydrogenated to oxaloacetate.
- Product Release: Oxaloacetate dissociates, regenerating the enzyme for subsequent catalytic cycles.
The reaction's reversibility allows MDH to participate in both ATP-generating (TCA cycle) and gluconeogenic pathways, depending on cellular energy demands.
Regulatory Dynamics
MDH activity is modulated by multiple physiological cues:
- Redox Coupling: Elevated NADH/NAD⁺ ratios suppress activity via feedback inhibition, preventing reductive stress and aligning flux with energetic needs. Low NADH levels enhance turnover, prioritizing malate oxidation during energy deficits.
- Substrate Availability: High malate concentrations drive oxaloacetate synthesis, sustaining TCA cycle progression. Accumulated oxaloacetate competitively inhibits MDH, ensuring metabolic equilibrium.
- Environmental Modulation:
- pH Sensitivity: Maximal activity occurs near pH 7.0–7.5, with acidic or alkaline conditions disrupting active site protonation states.
- Thermal Stability: Activity peaks at 35–40°C; temperatures exceeding 50°C induce irreversible denaturation.
Physiological and Biotechnological Relevance
- Metabolic Integration: MDH bridges glycolysis, TCA cycle, and gluconeogenesis, enabling carbon shuttling between mitochondria and cytosol. For example, maize ZmMdh4 gene mutant (mdh4-1) is characterized by small grains, low transparency, reduced starch content and significant accumulation of lysine. ZmMDH4, as cytoplasmic malate dehydrogenase, catalyzes the conversion of oxaloacetic acid (OAA) to malate, and its activity depends on the key glutamic acid (Glu) residue, which leads to the complete loss of enzyme function. Knocking down ZmMdh4 triggered endosperm metabolic reprogramming: glycolysis pathway was enhanced, mitochondrial complex I activity was disordered, ATP synthesis and respiratory chain balance were broken (Chen Y et al., 2020).
- Biomarkers: For example, the level of MDH1 in CSF of gCJD patients was detected by ELISA, and it was found that CSF-MDH1 in all patients with hereditary prion diseases (including E200K, V210I, P102L[GSS] and D178N[FFI] mutations) was significantly higher than that in the healthy control group, among which E200K and V210I mutation carriers were the most significantly higher (the diagnostic AUC was 0.87 and 0.85 respectively). Although the increase of MDH1 in patients with FFI and GSS is small, its correlation with common markers of neurodegeneration suggests that MDH1 can be used as a new auxiliary diagnostic marker of gCJD, especially in E200K/V210I subtype, which provides supplementary diagnostic value for the existing biomarker system (Zerr I et al., 2019).
References
- Chhimpa N, Singh N, Puri N, Kayath HP. "The Novel Role of Mitochondrial Citrate Synthase and Citrate in the Pathophysiology of Alzheimer's Disease." J Alzheimers Dis. 2023;94(s1):S453-S472. doi: 10.3233/JAD-220514
- Rajpurohit H, Eiteman MA. "Citrate synthase variants improve yield of acetyl-CoA derived 3-hydroxybutyrate in Escherichia coli." Microb Cell Fact. 2024 Jun 12;23(1):173. doi: 10.1186/s12934-024-02444-8
- Barrault M, Chabelskaya S, Coronel-Tellez RH, Toffano-Nioche C, Jacquet E, Bouloc P. "Staphylococcal aconitase expression during iron deficiency is controlled by an sRNA-driven feedforward loop and moonlighting activity." Nucleic Acids Res. 2024 Aug 12;52(14):8241-8253. doi: 10.1093/nar/gkae506
- Bancroft PJ, Turapov O, Jagatia H, Arnvig KB, Mukamolova GV, Green J. "Coupling of Peptidoglycan Synthesis to Central Metabolism in Mycobacteria: Post-transcriptional Control of CwlM by Aconitase." Cell Rep. 2020 Sep 29;32(13):108209. doi: 10.1016/j.celrep.2020.108209
- Grayson C, Faerman B, Koufos O, Mailloux RJ. "Fatty acid oxidation drives mitochondrial hydrogen peroxide production by α-ketoglutarate dehydrogenase." J Biol Chem. 2024 Apr;300(4):107159. doi: 10.1016/j.jbc.2024.107159
- Wang P, Mai C, Wei YL, Zhao JJ, Hu YM, Zeng ZL, Yang J, Lu WH, Xu RH, Huang P. "Decreased expression of the mitochondrial metabolic enzyme aconitase (ACO2) is associated with poor prognosis in gastric cancer." Med Oncol. 2013 Jun;30(2):552. doi:10.1007/s12032-013-0552-5
- Liu S, Cadoux-Hudson T, Schofield CJ. "Isocitrate dehydrogenase variants in cancer - Cellular consequences and therapeutic opportunities." Curr Opin Chem Biol. 2020 Aug;57:122-134. doi: 10.1016/j.cbpa.2020.06.012
- Piroli GG, Manuel AM, McCain RS, Smith HH, Ozohanics O, Mellid S, Cox JH, Cotham WE, Walla MD, Cascón A, Ambrus A, Frizzell N. "Defective function of α-ketoglutarate dehydrogenase exacerbates mitochondrial ATP deficits during complex I deficiency." Redox Biol. 2023 Nov;67:102932. doi: 10.1016/j.redox.2023.102932
- Tretter L, Adam-Vizi V. "Inhibition of Krebs cycle enzymes by hydrogen peroxide: A key role of [alpha]-ketoglutarate dehydrogenase in limiting NADH production under oxidative stress." J Neurosci. 2000 Dec 15;20(24):8972-9. doi: 10.1523/JNEUROSCI.20-24-08972.2000
- Lancaster MS, Kim B, Doud EH, Tate MD, Sharify AD, Gao H, Chen D, Simpson E, Gillespie P, Chu X, Miller MJ, Wang Y, Liu Y, Mosley AL, Kim J, Graham BH. "Loss of succinyl-CoA synthetase in mouse forebrain results in hypersuccinylation with perturbed neuronal transcription and metabolism." Cell Rep. 2023 Oct 31;42(10):113241. doi: 10.1016/j.celrep.2023.113241
- Wu B, Qiu J, Zhao TV, Wang Y, Maeda T, Goronzy IN, Akiyama M, Ohtsuki S, Jin K, Tian L, Goronzy JJ, Weyand CM. "Succinyl-CoA Ligase Deficiency in Pro-inflammatory and Tissue-Invasive T Cells." Cell Metab. 2020 Dec 1;32(6):967-980.e5. doi: 10.1016/j.cmet.2020.10.025
- Sebastian J, Hegde K, Kumar P, Rouissi T, Brar SK. "Bioproduction of fumaric acid: an insight into microbial strain improvement strategies." Crit Rev Biotechnol. 2019 Sep;39(6):817-834. doi: 10.1080/07388551.2019.1620677
- Chen Y, Xian M, Ying W, Liu J, Bing S, Wang X, Yu J, Xu X, Xiang S, Shao X, Cao J, He Q, Yang B, Ying M. "Succinate dehydrogenase deficiency-driven succinate accumulation induces drug resistance in acute myeloid leukemia via ubiquitin-cullin regulation." Nat Commun. 2024 Nov 13;15(1):9820. doi: 10.1038/s41467-024-53398-9
- Pecsi I, Hards K, Ekanayaka N, Berney M, Hartman T, Jacobs WR Jr, Cook GM. "Essentiality of succinate dehydrogenase in Mycobacterium smegmatis and its role in the generation of the membrane potential under hypoxia." mBio. 2014 Aug 12;5(4):e01093-14. doi: 10.1128/mBio.01093-14
- Kerins MJ, Milligan J, Wohlschlegel JA, Ooi A. "Fumarate hydratase inactivation in hereditary leiomyomatosis and renal cell cancer is synthetic lethal with ferroptosis induction." Cancer Sci. 2018 Sep;109(9):2757-2766. doi: 10.1111/cas.13701
- Chen Y, Fu Z, Zhang H, Tian R, Yang H, Sun C, Wang L, Zhang W, Guo Z, Zhang X, Tang J. "Cytosolic malate dehydrogenase 4 modulates cellular energetics and storage reserve accumulation in maize endosperm." Plant Biotechnol J. 2020 Dec;18(12):2420-2435. doi: 10.1111/pbi.13416
- Zerr I, Villar-Piqué A, Schmitz VE, Poleggi A, Pocchiari M, Sánchez-Valle R, Calero M, Calero O, Baldeiras I, Santana I, Kovacs GG, Llorens F, Schmitz M. "Evaluation of Human Cerebrospinal Fluid Malate Dehydrogenase 1 as a Marker in Genetic Prion Disease Patients." Biomolecules. 2019 Nov 28;9(12):800. doi: 10.3390/biom9120800