Glycolysis
In normal cells under ideal conditions, glucose enters the cell via glucose transporters (GLUT). Through the action of key glycolytic enzymes such as hexokinase (HK) and phosphofructokinase (PFK), glucose is broken down to produce pyruvate. Pyruvate then enters the mitochondria, where it is converted to acetyl-CoA. This acetyl-CoA is oxidized through the tricarboxylic acid (TCA) cycle, generating 30 or 32 molecules of ATP.
In hypoxic conditions, pyruvate cannot enter the mitochondria to be converted to acetyl-CoA. Instead, it is directly reduced to lactate, producing much less ATP.
In normal tissues, approximately 90% of ATP is generated via mitochondrial oxidative phosphorylation, while only about 10% of ATP comes from glycolysis. In contrast, in tumor cells, about 50% of ATP is synthesized through the glycolytic pathway.
The Role of Glycolysis in Cancer
Enhanced Glucose Uptake in Cancer Cells
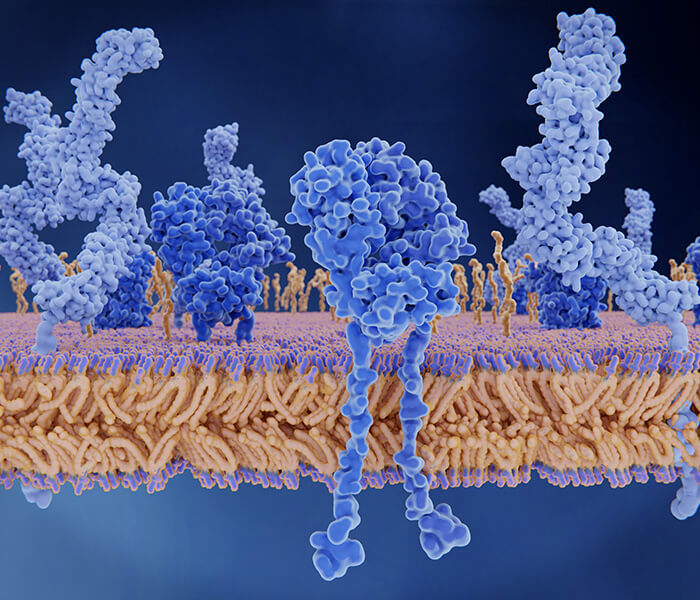
Cancer cells exhibit a distinctive metabolic phenotype characterized by their heightened demand for glucose, a phenomenon termed the "Warburg effect." This enhanced glucose uptake is facilitated by the upregulation of glucose transporters, particularly GLUT1, which enables cancer cells to scavenge glucose from the extracellular milieu at an accelerated rate. The overexpression of GLUT1 is commonly observed across various cancer types and is associated with poor prognosis and disease progression.
The increased glucose uptake serves as a fundamental metabolic adaptation that fuels the bioenergetic and biosynthetic demands of rapidly proliferating cancer cells. Glucose serves as a carbon source for various metabolic pathways, including glycolysis, the pentose phosphate pathway (PPP), and aerobic glycolysis, collectively supporting the synthesis of macromolecules essential for cell growth and division.
Increased Glycolytic Flux
Once inside the cell, glucose undergoes a series of enzymatic reactions within the glycolytic pathway to generate ATP and metabolic intermediates. Cancer cells exhibit an augmented glycolytic flux characterized by accelerated conversion of glucose to pyruvate, even under normoxic conditions. This hyperactive glycolytic phenotype is orchestrated by the dysregulation of glycolytic enzymes, such as hexokinase, phosphofructokinase, and pyruvate kinase, which are often overexpressed or post-translationally modified in cancer cells.
The preferential channeling of glucose-derived carbons into glycolysis provides cancer cells with a metabolic advantage by promoting rapid ATP production and facilitating the generation of glycolytic intermediates required for anabolic processes. Moreover, the diversion of glucose away from oxidative phosphorylation towards glycolysis promotes the shunting of glycolytic intermediates into biosynthetic pathways, supporting the production of lipids, nucleotides, and amino acids necessary for sustained cell proliferation.
Warburg Effect: Explanation and Significance
The Warburg effect, originally described by Otto Warburg in the 1920s, refers to the propensity of cancer cells to favor aerobic glycolysis as their primary metabolic pathway, even in the presence of oxygen. This metabolic reprogramming represents a departure from the conventional wisdom that oxidative phosphorylation is the predominant ATP-generating process in mammalian cells.
The Warburg effect confers several advantages to cancer cells, including:
- Rapid ATP production: Glycolysis enables cancer cells to generate ATP more quickly than oxidative phosphorylation, allowing for the rapid fulfillment of energy demands required for cell growth and division.
- Metabolic plasticity: By relying on glycolysis as the primary source of ATP, cancer cells exhibit metabolic flexibility that enables them to adapt to dynamic microenvironmental conditions, including fluctuations in oxygen and nutrient availability.
- Biosynthetic support: The diversion of glycolytic intermediates into anabolic pathways facilitates the biosynthesis of macromolecules, including nucleotides, amino acids, and lipids, necessary for cell proliferation and biomass accumulation.
The Warburg effect has profound implications for tumor biology and therapy, as it not only provides a metabolic advantage to cancer cells but also contributes to the remodeling of the tumor microenvironment. The increased production of lactate as a byproduct of glycolysis leads to the acidification of the extracellular milieu, creating a hostile environment that promotes tumor invasion, angiogenesis, and immune evasion.
Glycolytic Enzymes as Potential Therapeutic Targets
Given the critical role of glycolysis in fueling tumor growth and survival, enzymes involved in this pathway represent attractive targets for cancer therapy. Strategies aimed at inhibiting key glycolytic enzymes have shown promise in preclinical studies as a means of impairing cancer cell viability and suppressing tumor progression.
Hexokinase, the enzyme responsible for the phosphorylation of glucose to glucose-6-phosphate, is often overexpressed in cancer cells and plays a central role in regulating glycolytic flux. Inhibitors targeting hexokinase have been developed with the aim of disrupting glycolytic metabolism and inducing metabolic stress in cancer cells. Similarly, inhibitors targeting other glycolytic enzymes, such as phosphofructokinase and pyruvate kinase, have shown efficacy in preclinical models of cancer, highlighting the therapeutic potential of targeting glycolysis in cancer treatment.
However, the development of effective glycolysis-targeted therapies is challenged by the need for selective targeting to minimize off-target effects on normal tissues. Additionally, cancer cells exhibit metabolic plasticity and can adapt to glycolytic inhibition by upregulating alternative metabolic pathways to sustain their energy demands. Therefore, a deeper understanding of the metabolic vulnerabilities and adaptive responses of cancer cells is essential for the rational design of glycolysis-targeted therapies with improved efficacy and reduced toxicity.
Mechanisms Linking Glycolysis to Tumorigenesis
Hypoxia-Inducible Factor 1 (HIF-1) Activation
Hypoxia, or oxygen deprivation, is a hallmark of the tumor microenvironment resulting from inadequate blood supply due to rapid tumor growth and dysfunctional vasculature. Under hypoxic conditions, cells activate a transcriptional response mediated by hypoxia-inducible factor 1 (HIF-1), a heterodimeric transcription factor composed of HIF-1α and HIF-1β subunits. HIF-1 orchestrates a multitude of adaptive responses to hypoxia, including the upregulation of genes involved in glycolysis, angiogenesis, and cell survival.
In the context of tumorigenesis, HIF-1 activation promotes the metabolic reprogramming of cancer cells towards glycolysis, enabling them to thrive in the oxygen-deprived tumor microenvironment. HIF-1 induces the expression of key glycolytic enzymes, such as hexokinase, phosphofructokinase, and lactate dehydrogenase, thereby enhancing glycolytic flux and ATP production. Moreover, HIF-1-mediated upregulation of glucose transporters, particularly GLUT1, facilitates increased glucose uptake by cancer cells, further fueling glycolytic metabolism.
The activation of HIF-1 signaling not only promotes glycolysis but also contributes to other aspects of tumorigenesis, including tumor angiogenesis, metastasis, and resistance to therapy. HIF-1 induces the expression of vascular endothelial growth factor (VEGF), a potent angiogenic factor, promoting the formation of new blood vessels to supply oxygen and nutrients to the growing tumor. Additionally, HIF-1 activation enhances the expression of genes involved in epithelial-mesenchymal transition (EMT), facilitating tumor invasion and metastasis.
Oncogenes and Tumor Suppressors Regulating Glycolysis
Several oncogenes and tumor suppressors play critical roles in regulating glycolytic metabolism and contribute to the metabolic reprogramming observed in cancer cells. Oncogenic signaling pathways, such as the phosphatidylinositol 3-kinase (PI3K)/protein kinase B (AKT)/mammalian target of rapamycin (mTOR) pathway, promote glycolysis by enhancing glucose uptake and glycolytic enzyme expression.
Activation of the PI3K/AKT/mTOR pathway stimulates the translocation of GLUT1 to the plasma membrane, increasing glucose uptake by cancer cells. Moreover, AKT-mediated phosphorylation of glycolytic enzymes, such as hexokinase and phosphofructokinase, enhances their catalytic activity, further promoting glycolytic flux. Additionally, mTOR signaling promotes the translation of glycolytic enzymes through ribosomal protein S6 kinase (S6K) and eukaryotic translation initiation factor 4E (eIF4E) activation, reinforcing the glycolytic phenotype of cancer cells.
Conversely, tumor suppressor genes, such as p53, exert inhibitory effects on glycolysis to restrain tumor growth and proliferation. p53 regulates glycolytic metabolism through transcriptional regulation of key glycolytic genes, including GLUT1, phosphofructokinase, and lactate dehydrogenase. Activation of p53 suppresses glycolysis by inhibiting the expression of these glycolytic enzymes, promoting mitochondrial respiration, and enhancing oxidative phosphorylation.
The dysregulation of oncogenes and tumor suppressors contributes to the metabolic rewiring of cancer cells, promoting glycolytic metabolism and conferring a growth advantage in the tumor microenvironment.
Impact of Glycolytic Intermediates on Cell Signaling Pathways
In addition to its role in ATP production, glycolysis generates various metabolic intermediates that serve as signaling molecules to regulate cellular processes implicated in tumorigenesis. Accumulation of glycolytic intermediates, such as lactate, pyruvate, and acetyl-CoA, influences diverse signaling pathways involved in cell growth, survival, and metabolism.
Lactate, produced as a byproduct of glycolysis, functions as a signaling molecule that regulates immune cell function, angiogenesis, and tumor progression. High levels of lactate within the tumor microenvironment promote immune evasion by inhibiting the function of cytotoxic T cells and natural killer (NK) cells, impairing antitumor immune responses. Moreover, lactate promotes angiogenesis by stimulating the expression of VEGF and other pro-angiogenic factors, facilitating tumor vascularization and nutrient delivery.
Pyruvate, the end product of glycolysis, serves as a central node in cellular metabolism, linking glycolysis to other metabolic pathways, such as the tricarboxylic acid (TCA) cycle and amino acid metabolism. Pyruvate can be converted into acetyl-CoA, a precursor for de novo lipogenesis and cholesterol biosynthesis, supporting the increased demand for membrane synthesis in rapidly proliferating cancer cells.
Acetyl-CoA, derived from pyruvate metabolism, serves as a substrate for histone acetylation, an epigenetic modification that regulates gene expression and chromatin structure. Dysregulation of histone acetylation alters the transcriptional landscape of cancer cells, promoting tumorigenesis and therapeutic resistance. Moreover, acetyl-CoA links glycolytic metabolism to lipid biosynthesis, providing cancer cells with essential building blocks for membrane synthesis and energy storage.
Interaction Between Glycolysis and Other Metabolic Pathways
Glycolysis intersects with several other metabolic pathways, including the pentose phosphate pathway (PPP), amino acid metabolism, and lipid biosynthesis, to fulfill the diverse metabolic demands of proliferating cancer cells. Crosstalk between glycolysis and these pathways enables cancer cells to adapt to changing nutrient availability and metabolic stress, supporting their survival and proliferation in the tumor microenvironment.
The PPP, an alternative glucose metabolism pathway, generates NADPH and ribose-5-phosphate, essential for nucleotide synthesis and antioxidant defense, respectively. The PPP plays a critical role in maintaining redox balance and supporting biosynthetic processes in cancer cells, particularly under conditions of oxidative stress.
Amino acid metabolism is tightly linked to glycolysis, as glycolytic intermediates serve as precursors for amino acid synthesis through various biosynthetic pathways. Cancer cells exhibit increased demand for amino acids to support protein synthesis, cell proliferation, and redox regulation. Moreover, dysregulation of amino acid metabolism contributes to the rewiring of cancer cell metabolism, promoting tumorigenesis and therapeutic resistance.
Lipid biosynthesis is another essential metabolic pathway interconnected with glycolysis, providing cancer cells with lipids for membrane synthesis, energy storage, and signaling molecules. Glycolytic intermediates, such as acetyl-CoA and glycerol-3-phosphate, serve as substrates for de novo lipogenesis, fueling the increased demand for lipids in rapidly proliferating cancer cells.
The interaction between glycolysis and other metabolic pathways is orchestrated by a complex network of enzymes, transporters, and regulatory molecules, enabling cancer cells to adapt to dynamic metabolic conditions and sustain their growth and survival in the tumor microenvironment. Understanding the cross-talk between glycolysis and other metabolic pathways holds promise for identifying novel therapeutic targets and developing innovative strategies for cancer treatment.
 Differences in glycolysis pathways between normal cells and cancer cells (Kim et al., 2021).
Differences in glycolysis pathways between normal cells and cancer cells (Kim et al., 2021).
(A) In oxygen-rich conditions, normal cells generate up to 38 ATPs per glucose via glycolysis, the TCA cycle, and the electron transport system. In hypoxia, pyruvate accumulates, leading to lactic acid production and only 2 ATPs. (B) Cancer cells exclusively use glycolysis, yielding just 2 ATPs per glucose, necessitating more glucose for energy.
Glycolysis and Cancer Therapy
If we can regulate the activity of glycolytic enzymes in tumors and control the energy metabolism of these cells, we could inhibit tumor proliferation, leading to targeted therapy for malignant tumors. Consequently, researchers have been exploring methods to target the glycolytic pathway in cancer treatment. The enhanced glycolysis observed in tumor cells is primarily due to the increased expression or activity of key glycolytic enzymes. In recent years, efforts have been made to develop targeted therapies by inhibiting the activity of these critical enzymes in the glycolytic pathway.
Targeting Key Glycolytic Enzymes
Research indicates that inhibiting the glycolytic pathway in tumor cells can effectively suppress their proliferation and even induce cell death. Key glycolytic enzymes such as hexokinase 2 (HK2), phosphofructokinase (PFK), and pyruvate kinase M2 (PKM2) have emerged as tumor biomarkers. Their expression and activity significantly impact glycolysis in tumor cells, which in turn influences tumor growth.
- Hexokinase 2 (HK2)
HK2 catalyzes the first step in glycolysis, the phosphorylation of glucose to glucose-6-phosphate. This enzyme is often overexpressed in cancer cells, linking it closely to increased glycolytic activity. Inhibiting HK2 can disrupt this initial step, thereby hindering the entire glycolytic pathway and reducing the energy supply crucial for tumor growth.
- Phosphofructokinase (PFK)
PFK is another critical enzyme that regulates glycolysis by converting fructose-6-phosphate to fructose-1,6-bisphosphate. This enzyme's activity is tightly regulated and is often upregulated in cancer cells. Targeting PFK can effectively slow down glycolysis, thereby depriving cancer cells of energy and essential metabolic intermediates required for rapid proliferation.
- Pyruvate Kinase M2 (PKM2)
PKM2 plays a pivotal role in the final step of glycolysis, converting phosphoenolpyruvate to pyruvate. Unlike its isoforms, PKM2 is frequently expressed in cancer cells and is associated with promoting anabolic processes and cell growth. Inhibiting PKM2 can shift the metabolic balance, reducing the flow of glycolytic intermediates into biosynthetic pathways and impairing cancer cell growth.
Comprehensive Metabolic Targeting
While increased aerobic glycolysis is a hallmark of cancer cell metabolism, most cancer cells retain functional mitochondria and do not rely solely on glycolysis for energy production. Therefore, targeting the glycolytic pathway alone may not be sufficient. A comprehensive approach, understanding alternative metabolic pathways, is necessary for effective cancer therapy.
- Mitochondrial Metabolism
Cancer cells can adapt to glycolytic inhibition by increasing mitochondrial oxidative phosphorylation. Thus, targeting mitochondrial metabolism could be an effective complementary strategy. Inhibitors of the electron transport chain or mitochondrial biogenesis might be used in conjunction with glycolytic inhibitors to create a more robust anti-cancer strategy.
The PPP is crucial for generating NADPH and ribose-5-phosphate, essential for nucleotide synthesis and redox balance. Targeting the PPP can disrupt these processes, impairing the cancer cell's ability to manage oxidative stress and proliferate.
- Fatty Acid Synthesis
Cancer cells often exhibit increased fatty acid synthesis to support membrane formation and signaling. Inhibiting key enzymes involved in lipid biosynthesis, such as acetyl-CoA carboxylase (ACC) and fatty acid synthase (FASN), can limit the availability of essential lipids, reducing cancer cell growth and survival.
Cancer cells require a continuous supply of amino acids for protein synthesis and metabolic regulation. Targeting amino acid transporters and enzymes involved in amino acid biosynthesis and degradation can disrupt cancer cell metabolism. For example, inhibiting glutaminase, which converts glutamine to glutamate, can starve cancer cells of key substrates for energy production and biosynthesis.
- Tumor Acidification
The Warburg effect leads to increased production of lactate, causing acidification of the tumor microenvironment. This acidification promotes tumor invasion and suppresses immune responses. Targeting mechanisms that regulate pH in the tumor microenvironment, such as lactate transporters, can disrupt tumor growth and metastasis.
Reference
- Kim, So-Hee, and Kwang-Hyun Baek. "Regulation of cancer metabolism by deubiquitinating enzymes: The Warburg effect." International Journal of Molecular Sciences 22.12 (2021): 6173.