The one-carbon metabolic pathway constitutes a central biochemical network governing the mobilization and utilization of single-carbon groups (e.g., methyl, formyl, methylene). These units are indispensable for nucleotide biosynthesis, amino acid homeostasis, and methylation processes. At its core, folate derivatives and cobalamin (vitamin B₁₂) serve as enzymatic cofactors, orchestrating carbon unit transfer and transformation.
Metabolic Origins of Single-Carbon Units
- Serine-to-Glycine Conversion: SHMT catalyzes serine degradation to glycine, generating 5,10-methylene-THF (CH₂-THF).
- Glycine Cleavage System: Glycine undergoes mitochondrial cleavage via the GCS, yielding CO₂, NH₃, and CH₂-THF.
- Histidine Catabolism: Histidine degradation produces formiminoglutamate, which is enzymatically converted to CH₂-THF.
- Met Cycle: SAM-mediated methylation generates homocysteine (Hcy), which is remethylated to Met, sustaining the carbon flux.
Central Biochemical Reactions
Tetrahydrofolate (THF) acts as the primary scaffold for carbon unit shuttling, adopting distinct oxidation states:
- CH₂-THF: Supplies methylene groups for thymidylate synthesis (dTMP formation) and purine ring assembly (C8 position), directly impacting DNA replication fidelity.
- CHO-THF: Donates formyl units during purine biosynthesis (C2 position), essential for de novo nucleotide production.
- CH₃-THF: Facilitates homocysteine remethylation to methionine via vitamin B₁₂-dependent methionine synthase (MS), linking folate metabolism to epigenetic regulation through SAM-dependent methylation.
Pathway
The one-carbon metabolic network plays a vital role in cellular biochemical processes, facilitating the mobilization and utilization of single-carbon groups (e.g., methyl, formyl). This pathway underpins nucleotide synthesis, amino acid cycling, and methylation dynamics. Below, we delineate its core mechanisms, regulatory frameworks, and clinical implications.
Serine-Glycine Metabolic Axis
The serine-glycine-one-carbon axis serves as a metabolic linchpin, bridging nucleotide production, epigenetic regulation, and stress adaptation.
 The Serine-glycine biosynthesis pathway (Pan S et al., 2021).
The Serine-glycine biosynthesis pathway (Pan S et al., 2021).
Serine Conversion
- Reaction: Serine + THF → Glycine + 5,10-methylene-THF (CH₂-THF)
- Catalyst: Serine hydroxymethyltransferase (SHMT) operates in both cytosolic and mitochondrial compartments, with mitochondrial activity significantly contributing to energy homeostasis.
- Mechanism: SHMT transfers the β-carbon of serine to THF, generating glycine and CH₂-THF, a critical methyl donor for downstream processes.
Glycine Cleavage
- Reaction: Glycine + THF + NAD⁺ → CO₂ + NH₃ + CH₂-THF + NADH + H⁺
- Catalyst: Mitochondrial glycine decarboxylase complex (GCS) drives decarboxylation, yielding CH₂-THF for nucleotide biosynthesis and redox balance.
Metabolic Integration and Regulation
- Nucleotide Synthesis: CH₂-THF supplies methyl groups for thymidylate (dTMP) and purine (C8 position) formation, ensuring genomic integrity.
- Methylation Dynamics: CH₂-THF-derived 5-methyl-THF supports homocysteine remethylation to methionine, sustaining S-adenosylmethionine (SAM)-dependent epigenetic modifications.
Regulatory Influences
- Cofactor Availability: NAD⁺ levels modulate GCS activity, while NADH accumulation disrupts redox equilibrium.
- Nutrient Sensing: Cellular energy status and folate availability fine-tune SHMT and GCS enzymatic kinetics.
Pathophysiological Implications in Cancer
Anaplastic thyroid carcinoma (ATC) exemplifies the interplay between glutamine and one-carbon metabolism. Transcriptomic analyses reveal elevated expression of glutamine catabolism genes (GLS, SLC1A5) in ATC, supporting tumor proliferation under oxidative stress.Glutamine deprivation or GLS1 inhibition (via BPTES) reduces ATC growth but triggers compensatory upregulation of one-carbon genes (SHMT2, MTHFD2, PHGDH).ATF4 activation under glutamine stress enhances one-carbon pathway activity, promoting serine biosynthesis and redox adaptation.Co-targeting glutamine metabolism (e.g., GLS inhibitors) and one-carbon nodes (e.g., SHMT2 inhibitors), combined with antioxidants like Trolox, potentiates chemotherapy efficacy (e.g., lenvatinib).Comparative studies highlight heightened one-carbon dependency in ATC versus papillary thyroid carcinoma (PTC), correlating with aggressive phenotypes and poor prognosis. Murine models and patient datasets confirm that one-carbon gene overexpression aligns with therapeutic resistance and metastatic potential (Hwang Y et al., 2023).
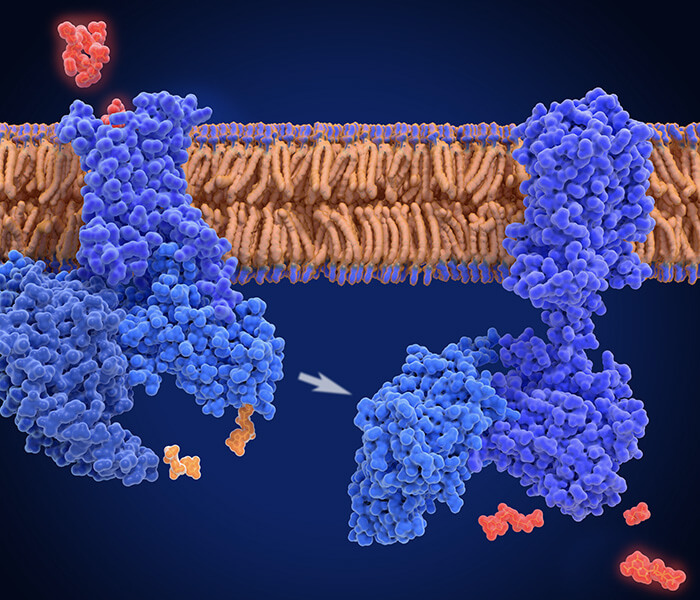
Thymidylate synthesis pathway
The thymidylate synthesis pathway is central to genomic replication and repair, ensuring adequate deoxythymidine monophosphate (dTMP) availability for DNA synthesis. This cytoplasmic process is particularly critical during cell division and damage response.
Biochemical Conversion of dUMP to dTMP
Catalytic Mechanism
- Thymidylate synthase (TS) mediates the transfer of a methylene group from 5,10-methylene-THF (CH₂-THF) to deoxyuridine monophosphate (dUMP), yielding dTMP—a pyrimidine essential for DNA strand elongation.
- Enzyme Dynamics: TS exhibits sequential substrate binding, with dUMP (Kd=0.5 μM) docking prior to CH₂-THF, inducing conformational activation.
- Pharmacological Inhibition: The antimetabolite 5-fluorouracil (5-FU) irreversibly inhibits TS (Ki=0.1 nM), mimicking dUMP to disrupt nucleotide balance.
Dihydrofolate Reductase (DHFR) Function
- DHFR regenerates tetrahydrofolate (THF) from dihydrofolate (DHF) using NADPH as a reductant, sustaining CH₂-THF pools.
- Therapeutic Targeting: Methotrexate (MTX) competitively binds DHFR (IC₅₀=1 nM), depleting THF and halting DNA synthesis.
Regulatory Circuits
- Feedback Control: Elevated dTMP concentrations allosterically suppress TS activity, preventing overproduction.
- Cofactor Limitation: THF scarcity restricts CH₂-THF generation, directly throttling dTMP synthesis.
- Clinical Interventions:
- TS Inhibitors: 5-FU and derivatives impede dTMP production, selectively targeting rapidly dividing cells.
- DHFR Antagonists: MTX and pemetrexed disrupt folate cycling, augmenting chemotherapeutic efficacy.
Methodological Advancements
- Kinetic Profiling: ³H-dUMP Incorporation Assays: Quantify dTMP synthesis rates via radioisotope tracing.
- Metabolite Quantification: Isotope dilution LC-MS/MS with ¹³C5-dTMP internal standards achieves attomolar sensitivity.
Pathophysiological Implications
- Inadequate folate intake correlates with elevated colorectal cancer (CRC) risk, as suboptimal dTMP pools increase DNA replication errors.Reduced SHMT1 expression in Apc<sup>min/+</sup> mice downregulates thymidylate synthase (TYMS) and thymidine kinase 1 (TK1), impairing dTMP synthesis without altering methylation or purine pathways. Folate deficiency exacerbates DNA strand breaks in Apc-heterozygous models, synergizing with Shmt1 dysregulation to accelerate intestinal tumorigenesis.SHMT1 modulates TYMS/TK1 levels, positioning it as a biomarker for CRC susceptibility and a target for metabolic intervention (Macfarlane AJ et al., 2011).
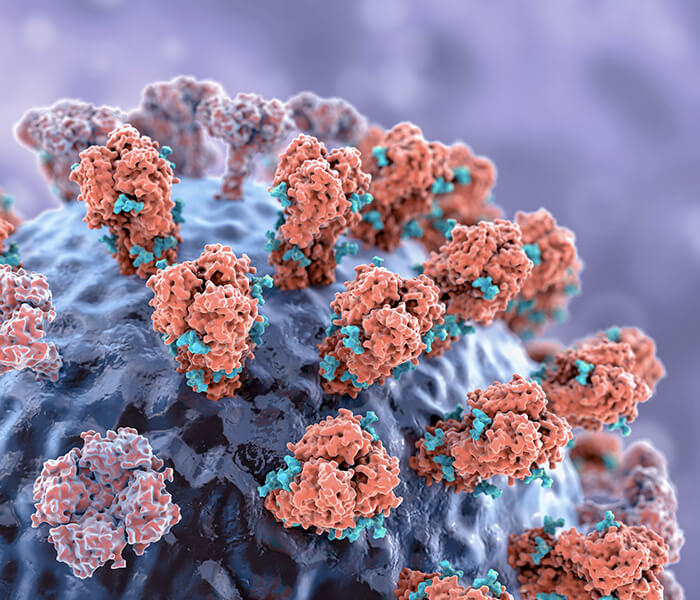
Purine synthesis pathway
Purine is synthesized by de novo pathway or by using existing purine nucleotides (such as adenine and guanine). In the de novo pathway, purine synthesis starts with simplified precursor molecules (such as carbamoyl phosphate), and carbon and nitrogen sources are gradually added to form purine nucleotides.
CHO-THF and CH=THF play an important role in purine synthesis. They provide C2 and C8 positions respectively and participate in the synthesis of purine ring structure.
 De novo and salvage purine synthesis pathways in mammals (Mizukoshi T et al., 2023).
De novo and salvage purine synthesis pathways in mammals (Mizukoshi T et al., 2023).
Key reactions and enzymes in purine synthesis
C2 site synthesis reaction
- Reaction: 5- aminoimidazole -4- carboxamide nucleotide (AICAR)+CHO-THF generates 5- carboxamide imidazole -4- carboxamide nucleotide (FAICAR).
- Enzyme: AICAR formyl transferase.
- Location: Cytoplasm. Aichar formyltransferase catalyzes this reaction, and the formyl group in CHO-THF is transferred to the 5- aminoimidazole -4- formamide part of Aichar.
- C2 (formyl): from 10- formyl -THF, catalyzed by formyltransferase (ATIC).
C8 site synthesis reaction
- Reaction: GAR+CH=THF generates FGAR.
- Enzyme: GAR formyltransferase.
- Location: Cytoplasm. GAR formyltransferase catalyzes the reaction, and the methylene formyl group in CH=THF is transferred to the C8 position of GAR.
- C8 (methylene): Catalyzed by GART and dependent on 5,10- methylene -THF.
Optimization of experimental methods
- Isotope tracing: C-glycine labeling is used to trace the carbon sources at C4, C5 and C7 of purine ring.
- Enzyme activity detection: for example, determine the amount of FGAR produced by HPLC (retention time =8.2 min, C18 column).
Physiological significance
- Abnormal metabolism will affect DDR and lead to cancer: HCC is a common type of liver cancer with high mortality. It is found that purine metabolism in HCC is out of balance, and the activation of de novo purine biosynthesis may be related to tumor growth, the imbalance of DNA damage repair mechanism and the fragility of treatment. Through the analysis of HCC cell line, it is found that hyperpurine anabolism is related to DDR targeted drugs (such as ATR inhibitor berzosertib) and better response to radiotherapy. In terms of non-DDR targeted drugs, hyperpurine anabolism is related to drug resistance. Cell line SNU475 (with the lowest purine anabolism) is highly sensitive to sorafenib and regofinib, two HCC targeting drugs. For drugs that interfere with the repair of double-stranded DNA breaks (such as berzosertib and mitoxantrone), cells with high purine anabolism are more sensitive to these drugs, while SNU475 cells show drug resistance.For targeted drugs of single-stranded DNA repair pathway (such as Olapani, etc.), these drugs failed to significantly cause cytotoxicity in all HCC cell lines.Berzosertib is an ATR inhibitor, and it has been found that it has stronger cytotoxicity in HCC cells with high purine anabolism. By detecting r-H2AX signal transduction in different cell lines, it is proved that berzosertib can induce DNA damage. Inhibition of purine anabolism (such as ATIC gene knockout) weakens the cytotoxicity of berzosertib, while enhancement of purine anabolism (such as ATIC overexpression) increases the sensitivity of cells to berzosertib. M6A modification is related to purine anabolism in HCC, and promotes tumor genome instability by affecting the transcriptome changes of DDR gene, which may be one of the reasons why HCC cells are more sensitive to DDR targeted drugs. Purine anabolism may be used as a biomarker to predict the response of HCC patients to DDR inhibitors (such as berzosertib) or other treatments (such as TACE) (Hung MH et al., 2023).
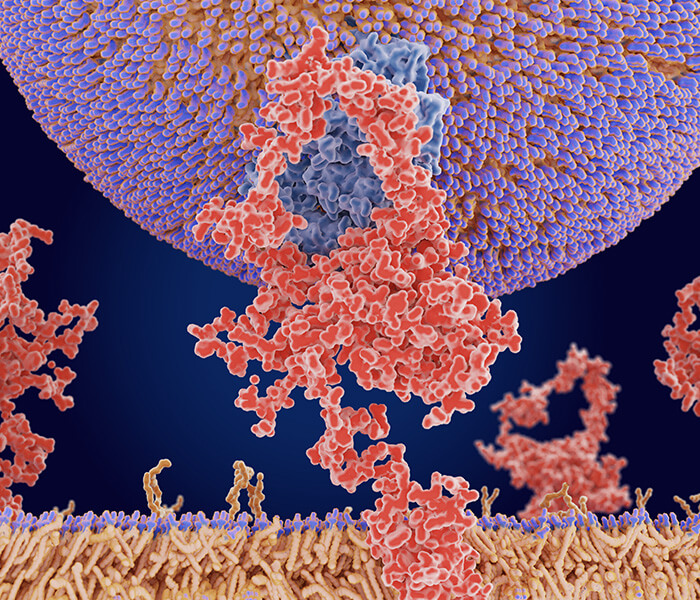
Methionine cycle
The methionine cycle is a fundamental biochemical network governing methyl group transfer and regeneration, essential for epigenetic regulation, protein function, and cellular homeostasis. This pathway cycles homocysteine (Hcy), methionine (Met), and S-adenosylmethionine (SAM) through interconnected reactions, directly influencing gene expression, DNA repair, and metabolic adaptation.
 Overview of one-carbon metabolism around the folate cycle, methionine cycle and trans-sulfuration pathway (Pan S et al., 2021).
Overview of one-carbon metabolism around the folate cycle, methionine cycle and trans-sulfuration pathway (Pan S et al., 2021).
Core Biochemical Reactions
Homocysteine Remethylation
- Reaction: Hcy + 5-methyl-THF → Met + THF
- Catalyst: Vitamin B₁₂-dependent methionine synthase (MS) facilitates methyl transfer from 5-methyl-THF to Hcy in the cytoplasm.
- Cofactor Dependency: Vitamin B₁₂ acts as a methyl carrier, ensuring efficient Met regeneration.
- Reaction: Met + ATP → SAM + PPi + Pi
- Catalyst: Methionine adenosyltransferase (MAT) conjugates Met with ATP, yielding SAM—the universal methyl donor—in cytoplasmic compartments.
Methylation Reactions
- Process: SAM transfers methyl groups to DNA, histones, and proteins via methyltransferases (e.g., DNMTs, HMTs), modulating chromatin states and cellular signaling.
- Byproduct: S-adenosylhomocysteine (SAH) is hydrolyzed by SAHH to regenerate Hcy and adenosine, completing the cycle.
Regulatory Mechanisms
- SAM/SAH Homeostasis: A ratio >5 sustains methylation capacity; values <2 (e.g., in cirrhosis) indicate impaired potential.
- Vitamin B₁₂ Deficiency: Traps folate as 5-methyl-THF, disrupting nucleotide synthesis and causing megaloblastic anemia.
Methodological Innovations
- LC-MS/MS Quantification: Synchronous measurement of SAM/SAH (LOQ=0.1 nM) using 0.1% formic acid-methanol gradients.
- Pyrosequencing: Targets LINE-1 repeats to assess genome-wide methylation levels.
Therapeutic and Pathological Insights
- Histidine impacts gut microbiota and liver health by serving as a key energy source for microbiota and exerting a scavenging effect on the host. In the context of non-alcoholic fatty liver disease (NAFLD), plasma histidine levels are strongly and negatively correlated with hepatic steatosis, as well as with specific gene profiles in the hepatic transcriptome, such as those related to insulin signaling, inflammation, and trace amine-associated receptor 1 (TAAR1). Circulating histidine levels are negatively correlated with certain bacterial groups, like Proteobacteria, and positively correlated with bacteria that lack histidine utilization systems.The study initially analyzed genes associated with plasma levels of hs-CRP, glucose, and triglycerides (TG), and through Reactome pathway enrichment analysis, it was found that histidine acts through different genes and pathways compared to those associated with these metabolic factors. In experiments involving human primary hepatocytes, histidine amide (HAA) supplementation modulated metabolic processes such as lipogenesis and β-oxidation, and increased the expression of fatty acid transport and anti-inflammatory genes, particularly the TAAR1 gene.In mouse experiments, HAA supplementation reduced key features of NAFLD, including improving liver fat deposition, lowering liver fat levels, reducing inflammation, and enhancing insulin sensitivity. The effects of HAA supplementation were also validated in genetic (ob/ob) mice and surgical (ovariectomized OVX) rat models. The results showed that HAA supplementation significantly alleviated hepatic steatosis, reduced the expression of lipogenesis-related genes, promoted the proliferation of beneficial flora (e.g., Lactobacillaceae), and reduced harmful flora abundance, while also reducing inflammation.Macrogenomic analysis revealed a negative correlation between circulating histidine levels and members of the intestinal Proteobacteria, as well as a positive correlation with beneficial bacteria such as Cyanobacteria, Actinobacteria, and Bifidobacteria. Additionally, the abundance of histidine utilization-related genes (e.g., hutH, hutU, hutI, and hutG) was found to correlate with the degree of hepatic steatosis (Quesada-Vázquez S et al., 2023).
Histidine metabolism
Histidine metabolism is an important part of AA metabolism, and its degradation process not only helps to maintain the balance of amino acids, but also involves the synthesis of some key metabolites, such as iminomethylglutamic acid and CH₂-THF.
Conversion of histidine to iminomethylglutamic acid
- Reaction: histidine→ iminomethylglutamic acid.
- Enzyme: Histidine Ammonia-Lyase (HAL).
- Location: Cytoplasm.
- Reaction principle: histidine ammonia lyase catalyzes the deamination reaction of histidine and converts histidine into iminomethylglutamic acid (also known as 1- methylhistidine). This reaction will release ammonia (NH) and produce iminomethylglutamic acid. Histidine not only exists as an important bioactive molecule in the body (for example, as a precursor of neurotransmitters), but also participates in the removal of ammonia and the conversion of amino acids during metabolism.
- Biological significance: The degradation of histidine plays an important role in eliminating excess amino acids in the body and regulating the concentration of ammonia. Especially in organs such as the liver, this process helps to avoid the accumulation of ammonia, thus maintaining the nitrogen balance in the body.
The conversion of iminomethylglutamic acid into CH₂-THF
- Reaction: Iminomethylglutamic acid+THF → glutamic acid+CH₂-THF.
- Enzyme: Formiminotransferase.
- Location: Cytoplasm.
- Reaction principle: Iminomethyltransferase catalyzes the transfer reaction between iminomethylglutamic acid and THF. THF accepts imino group from iminomethylglutamic acid and converts it into CH₂-THF. In this process, thf is a methyl donor and participates in the methylation reaction.
Metabolic pathway
- Histidine → glutamic acid: Iminomethylglutamic acid is generated through four-step reaction, which contributes one carbon unit to THF cell.
- Tissue specificity: the liver is the main site of histidine degradation, and the contribution in brain tissue can be ignored.
Optimization of experimental methods
- Metabolite detection: for example, iminomethylglutamic acid will be derivatized into dansyl chloride compound, and fluorescence detection (Ex/Em=340/520 nm).
- Determination of enzyme activity: for example, detection of iminomethyltransferase, coupled with NADPH consumption (absorbance decreased at 340 nm), detection of CH₂-THF production.
Histidine metabolism is not limited to the above two-step reaction, and its metabolites can also be intertwined with many important metabolic pathways.
Services You May Be Interested In:
Additional Resources:
Physiological significance
- Impacts gut microbiota and thus liver health: histidine acts as a key energy source for the microbiota and has a scavenging effect on the host. In the context of NAFLD, plasma histidine is strongly negatively correlated with hepatic steatosis, as well as with specific gene profiles in the hepatic transcriptome (e.g., insulin signaling, inflammatory response, and trace amine-associated receptor 1). Circulating histidine levels were negatively correlated with certain groups of bacteria (e.g., Proteobacteria) and positively correlated with bacteria lacking histidine utilization systems. The study first analyzed genes associated with plasma hs-CRP, glucose, and triacylglycerol (TG) levels and found, by Reactome pathway enrichment analysis, that histidine acts differently from the genes and pathways associated with these metabolic factors. In experiments with human primary hepatocytes, HAA supplementation modulated metabolic processes such as lipogenesis and β-oxidation, and increased the expression of fatty acid transport and anti-inflammatory genes, particularly the TAAR1 gene. Experiments with HAA supplementation in mice revealed that the supplementation reduced key features of NAFLD, including improving fat deposition in the liver, lowering liver fat levels, reducing inflammation, and improving insulin sensitivity. The study also validated the effects of HAA supplementation in a genetic mouse model (ob/ob mice) and a surgical rat model (ovariectomized OVX rats). The results showed that HAA supplementation significantly ameliorated hepatic steatosis, reduced the expression of lipogenesis-related genes, promoted the proliferation of beneficial flora (e.g., Lactobacillaceae), and reduced the abundance of harmful flora, as well as reduced inflammatory responses. Macrogenomic analysis by birdshot revealed a negative correlation between circulating histidine levels and members of the intestinal Proteobacteria, and a positive correlation with some other beneficial flora (e.g., Cyanobacteria, Actinobacteria phylum, Bifidobacteria spp.). In addition, the abundance of histidine utilization-related genes (e.g., hutH, hutU, hutI, and hutG) was found to correlate with the degree of hepatic steatosis (Quesada-Vázquez S et al., 2023).
Folic acid cycle
Folic acid cycle mainly involves THF and its derivatives, providing a carbon unit (methyl, methylene, etc.) to support a variety of biochemical reactions. This cycle is the core of the intracellular carbon metabolism network, and the reactions involved are very important for DNA synthesis, repair, methylation and AA metabolism.
Key steps of folic acid cycle
- Synthesis of THF: Folic acid itself (vitamin B) needs to be reduced to THF, which is the initial step of folic acid cycle. THF is an active form that can accept and transfer one carbon unit.
- The transfer of one carbon unit: THF can bind and transfer different forms of one carbon unit. Common forms include -CH and -CH-. Through these reactions, THF is derived into many different forms, such as 5-ch-THF, 5,10-ch-THF and so on.
- Participate in methylation reaction: 5-CH-THF in folic acid cycle is an important methyl donor, which provides methyl groups when Hcy is converted into Met. Met can then be converted into SAM, which participates in the Me of DNA, RNA and protein.
- Relationship with Hcy metabolism: 5-CH-THF forms Met by transferring methyl to Hcy.
Summary
Folic acid cycle widely affects many other metabolic pathways by providing key one carbon unit, including:
- Serine-glycine cycle: providing one carbon unit to participate in the synthesis of 5,10- CH₂-THF.
- Synthesis of thymidylate: 5,10-CH₂-THF provides methyl for the synthesis of thymidylate.
- Purine synthesis: 5,10-CH₂-THF provides one carbon unit and participates in purine synthesis.
- Met cycle: 5-CH₂-THF provides methyl for the conversion of Hcy to Met.
- Histidine metabolism: one carbon unit of folic acid cycle affects the metabolism of histidine and other amino acids.
References
- Reina-Campos M, Diaz-Meco MT, Moscat J. "The complexity of the serine glycine one-carbon pathway in cancer." J Cell Biol. 2020 ;219(1):e201907022. doi: 10.1083/jcb.201907022
- Mizukoshi T, Yamada S, Sakakibara SI. "Spatiotemporal Regulation of De Novo and Salvage Purine Synthesis during Brain Development." eNeuro. 2023;10(10):ENEURO.0159-23.2023. doi: 10.1523/ENEURO.0159-23.2023
- Hwang Y, Yun HJ, Jeong JW, Kim M, Joo S, Lee HK, Chang HS, Kim SM, Fang S. "Co-inhibition of glutaminolysis and one-carbon metabolism promotes ROS accumulation leading to enhancement of chemotherapeutic efficacy in anaplastic thyroid cancer." Cell Death Dis. 2023;14(8):515. doi: 10.1038/s41419-023-06041-2
- Macfarlane AJ, Perry CA, McEntee MF, Lin DM, Stover PJ. "Shmt1 heterozygosity impairs folate-dependent thymidylate synthesis capacity and modifies risk of Apc(min)-mediated intestinal cancer risk." Cancer Res. 2011 ;71(6):2098-107. doi: 10.1158/0008-5472.CAN-10-1886
- Hung MH, Chang CW, Wang KC, Chaisaingmongkol J, Ruchirawat M, Greten TF, Wang XW. "Purine anabolism creates therapeutic vulnerability in hepatocellular carcinoma through m 6 A-mediated epitranscriptomic regulation." Hepatology. 2023 ;78(5):1462-1477. doi: 10.1097/HEP.0000000000000420
- Peng H, Yan Y, He M, Li J, Wang L, Jia W, Yang L, Jiang J, Chen Y, Li F, Yuan X, Pang L. "SLC43A2 and NFκB signaling pathway regulate methionine/cystine restriction-induced ferroptosis in esophageal squamous cell carcinoma via a feedback loop." Cell Death Dis. 2023 ;14(6):347. doi: 10.1038/s41419-023-05860-7
- Quesada-Vázquez S, Castells-Nobau A, Latorre J, Oliveras-Cañellas N, Puig-Parnau I, Tejera N, Tobajas Y, Baudin J, Hildebrand F, Beraza N, Burcelin R, Martinez-Gili L, Chilloux J, Dumas ME, Federici M, Hoyles L, Caimari A, Del Bas JM, Escoté X, Fernández-Real JM, Mayneris-Perxachs J. "Potential therapeutic implications of histidine catabolism by the gut microbiota in NAFLD patients with morbid obesity." Cell Rep Med. 2023 ;4(12):101341. doi: 10.1016/j.xcrm.2023.101341